- Citas Centro Médico de Caracas: Lunes, Miercoles y Viernes. Pulse el botón Agende una Cita
- Sistema de citas en linea exclusivo para Centro Medico de Caracas en San Bernardino
- Citas CMDLT: Jueves. llamar al 0212-9496243 y 9496245
- Las Emergencias son atendidas en CMDLT previa coordinacion personal al 04142708338
- Proveedor Seguros Mercantil y Sudeban
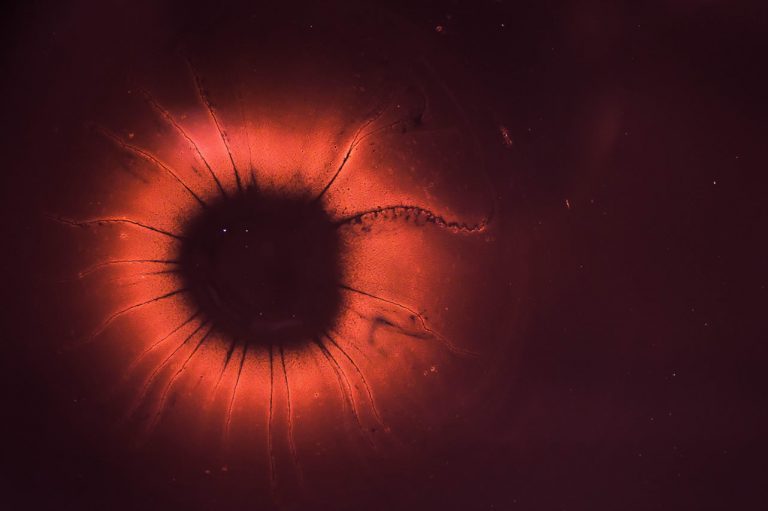
This is a condition in which the placenta is implanted in an abnormally low location in the gravid uterus, below the baby and in relation to the internal cervical os.
If we imagine the pregnant uterus as a balloon inflated with air we observe that there are two basic parts, the body and the neck. The body represents the most voluminous part of the globe and the one that makes it look like a ball. The neck is the tubular portion where we knot so that the air does not escape (channel), which we use to inflate (external orifice) and whose inner end communicates with the body of the balloon (internal orifice). This internal orifice is the one that represents for us obstetricians the point of reference to determine the presence of a placenta previa.
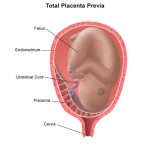
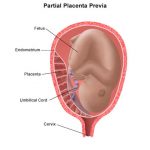
Normally the placenta inserts and develops away from the internal hole of the cervix but occasionally we discover that the placenta is abnormally low and close to the margins of this hole and even over it, partially or totally occluding it: hence the placement of Insertion Placenta low, marginal placenta, partial prenatal placenta and total prenatal placenta or center-occlusive. The greater the degree of obstruction, the greater the symptomatology and severity of the clinical picture.
How does this happen?
Placenta previa occurs when the fertilized egg is implanted in the lower portion of the uterus instead of the usual and adequate upper position. It is suggested that this occurs when there are some damage to the uterine cavity (repeated cesareans, curettage and uterine infections) that lead to the placenta being inserted in less altered places such as the lower surfaces of the uterus.
We reserve the term placenta previa for after 20 weeks of pregnancy since any bleeding at this time would be called a threat of abortion and not otherwise; in fact, a loss before 20 weeks of pregnancy would be classified as an abortion. Up to 15% of pregnant women show some category of placenta previa before 20 weeks and of these only a very small fraction will become a true pre-pregnancy. For safety reasons when diagnosing Placenta Previa before week 20 I take preventive measures to avoid bleeding that could lead to an abortion.
Some women present a greater risk than others and it is known that in the following conditions it is more frequent to observe the problem
- Women over 35 years old
- Women smokers and users of cocaine
- Multiparous
- Women who have aborted several times, multiple uterine curettages (curettage)
- Women who have had more than one cesarean
- Women who have had Placenta Previously.
What is the importance of this anomaly?
Imagine that at the time of delivery, the baby can not be born because there is an obstacle that prevents him from leaving the uterus to the outside, through the vagina; Thus, the presence of a Placenta Previa prevents a normal delivery while generating other problems of great importance and danger to the mother and her baby, Hemorrhage and Prematurity. When the placenta is located very close, or over the internal cervical os, its local fixation to the uterus is very unstable and there may be small detachments of the placental border that expose some uterine vessels, which will produce a hemorrhage of variable magnitude, from small spots to a clear vaginal hemorrhage with potential to bleed to the mother. On the other hand, the blood acts as a uterine irritant and can stimulate painful uterine contractions that contribute to greater placental detachments and greater bleeding, thus reestablishing a vicious circle that can lead to an obstetric emergency. If the bleeding begins to manifest when the pregnancy is preterm (before week 37) and does not respond to medical management, we need to interrupt the pregnancy with an emergency caesarean section and obtain a premature baby that will need intensive care. If this happens at the end of pregnancy, the situation is better for the baby because although we have to perform an emergency caesarean section, the baby is unlikely to require intensive therapy.
Who bleeds: the mother or the fetus?
Bleeding is of maternal origin and in most cases is discrete and allows us to handle the situation conservatively, at least initially. Fortunately, severe cases are relatively infrequent but dangerous for the mother because a profuse and uncontrollable hemorrhage can generate severe secondary complications.
What are the symptoms?
As will be seen later, the classic symptom is a bright, painless red vaginal bleeding with no apparent triggering cause. Sex, intense physical exercise or weight bearing can be triggers.
How to diagnose?
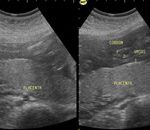
Early diagnosis is echographic, and we can diagnose 100% of these cases using modern high-resolution equipment before the symptoms appear, and this should be in most cases, if there is adequate prenatal control . Once the bleeding has begun, the clinical evaluation suggests the problem and the ultrasound confirms its presence.
Early or Asymptomatic Diagnosis: when the mother controls her pregnancy, we make the diagnosis before the symptoms appear and we can suggest preventive measures to avoid bleeding in the future. In precocious pregnancies we diagnose this condition in 7% of pregnant women but they will manifest the problem only 0.5%. This is because as the pregnancy progresses and the uterus grows, the placenta, which initially was “low” is ascending and moving away from the internal cervical os. This is the reason why we do not use the diagnosis of Placenta Previa before the 20th week of pregnancy, we usually report the condition as a “low” placenta so that the obstetrician is aware of a potential problem and makes an adequate follow-up.
Late or Symptomatic Diagnosis: typically the patient consults with a pregnancy greater than 20 weeks presenting painless vaginal bleeding that started without reason or apparent cause. The hemorrhage is usually unexpected, although initially it presents as a discrete spotting there is a tendency to recurrence days or weeks later and in increasing amounts. The movements of the baby are normal and the patient feels well except for the concern that causes vaginal bleeding (if the bleeding has been profuse may manifest weakness, dizziness, palpitations). Painful uterine contractions may be associated with bleeding. In no way do we perform a gynecological touch (this could cause a greater bleeding) and in selected cases we place a speculum to determine the intrauterine origin of the bleeding. Immediately the patient is transferred to the Ultrasound Room for the definitive diagnosis.
Prediction: The anterior placenta previa (anterior aspect of the uterus) has a greater possibility of normalizing than the posterior placentae.
Sonographers are suggested to report in millimeters the relation of the placenta to the internal cervical orifice of the uterus: distance from the placental edge to the internal orifice or measurement of its superposition past said orifice.
The presence of the edge of the placenta exactly over the hole is a 0 mm or marginal placenta.
If the placenta is marginal or overlaps more than 15 mm above the cervical os during week 18-24 re evaluation of the placenta is suggested after week 26 and some risk of placenta previa can be predicted at the end of pregnancy.
If the placental border is more than 20 mm past the internal cervical os (previous occlusal center) after week 26 the placenta previa condition is final and a cesarean section will be required
Oppenheimer L, Society of Ob / Gyn Canada. Diagnosis and management of placenta previa. J Obstet Gynaecol Can 2007 Mar; 29 (3): 261-6.
Which is the treatment?
The treatment of this condition depends on the age of the pregnancy and the magnitude of the mother’s bleeding. The genital bleeding and the possibilities of its management deprive on the gestational age of pregnancy, the priority is always the mother and if saving the life of the mother requires an emergency caesarean in a preterm pregnancy, this is carried out without any doubt.
Pregnancy less than 37 weeks without vaginal bleeding (asymptomatic):
- Ambulatory expectant management
- Prenatal check every 1-2 weeks
- Ultrasound every 1-4 weeks
- Sexual abstinence (absolute), the use of tampons is contraindicated
- Relative rest at home, frequent bed rest
- Measures of lung maturation
Pregnancy less than 37 weeks in the presence of bleeding (symptomatic):
Hospitalization during each episode of bleeding is a possibility
- Absolute bed rest, absolute prohibition of sexuality and vaginal manipulation
- The use of vaginal tampons is strictly prohibited
- Frequent echoes every 1-2 weeks if bleeding stops
- Pharmacological measures of lung maturation
- Medications to stop uterine contractions
- Iron orally and blood transfusions if necessary
- Cesarean section if necessary.
Pregnancy greater than or equal to 37 weeks with or without bleeding:
- Maintain the indicated type of rest until obstetric behavior is decided
- Ecosonography to verify fetal age and health
- Interruption of pregnancy: the definitive treatment of this condition is the birth of the baby.
Since the bleeding is unpredictable, and its consequences an emergency, it is customary to interrupt the pregnancy once the fetal maturity has been verified before spontaneous labor begins: the cervical dilatation detaches the placenta, triggering profuse bleeding.
Placenta Previa
Graphics courtesy of WebMD
Prevention
There is not really an effective prevention, in fact, you can not prevent the occurrence of Placenta Previa, you can only limit its effects once the problem has been diagnosed. Although it does not serve as a specific preventive measure, you should consider maintaining a healthy and active life, avoiding excessive use of alcohol and stopping the use of cigarettes and drugs.
Care
- Follow to the letter the instructions that your doctor has made for your case and particular gestational age, including medication use and restrictions on physical, sexual and domestic activity (rest may be less strict if the condition has remained asymptomatic, but sexuality is always forbidden)
- If you go to another doctor, immediately notify the presence of your placental condition so that you do not have a vaginal touch or place a speculum if the center does not have the right conditions to attend a hemorrhagic obstetric emergency.
- Immediately report any degree of vaginal bleeding, uterine contractions and alteration of your baby’s movements.
Diagnosis and prognosis
Of all the diagnoses that are made of Placenta Previa (up to 7 of every 100 pregnancies) only 0.5% will be a real and definitive case.
When the first bleeding occurs before week 32, the fetal prognosis is reserved because the immediate termination of pregnancy and obtaining a premature baby may be required. Immediate rest can stop the progression. Repetitive genital bleeding can compromise maternal health.
When the first bleeding occurs after week 33, the prognosis is better because we are getting closer to fetal maturity and there is less time to wait for repeated bleeding.
Repeated bleeding leads to the termination of pregnancy, usually we tolerate 2 or 3 episodes of small amount, by making more frequent and intense pregnancy is interrupted via emergency cesarean section. The hemorrhagic complications in pregnancy consume platelets and coagulation factors so the patient can reach a state of blood incoagulability that can endanger her life, this is the reason why we do not tolerate many hemorrhagic episodes.