- Citas Centro Médico de Caracas: Lunes, Miercoles y Viernes. Pulse el botón Agende una Cita
- Sistema de citas en linea exclusivo para Centro Medico de Caracas en San Bernardino
- Citas CMDLT: Jueves. llamar al 0212-9496243 y 9496245
- Las Emergencias son atendidas en CMDLT previa coordinacion personal al 04142708338
- Proveedor Seguros Mercantil y Sudeban
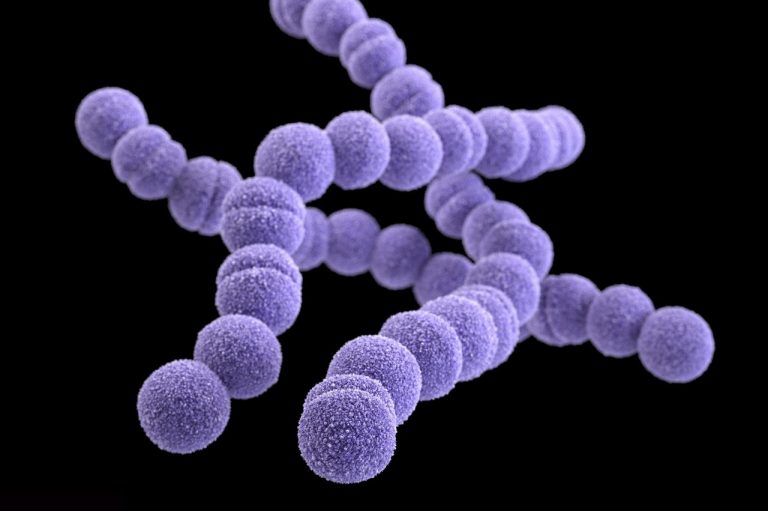
Group B Streptococcus (GBS, Streptococcus agalactiae) is a bacterium known to veterinarians as a cause of mastitis in dairy cattle that leads to a lack of milk production (hence the name agalactiae, without milk). In 1934 it was described as causing 3 cases of maternal death due to puerperal fever and later its association with the Newborn infection and sepsis / neonatal death was discovered.
This germ colonizes the anovulvar region asymptomatically in healthy women (10-30%) and being a less aggressive bacterium rarely causes infections outside of pregnancy or postpartum period. However, for the Newborn is another story, due to its immunological immaturity contamination with this agent leads to a severe infection that endangers your life.
Since the 90s guidelines have been established to detect and correctly manage the maternal presence of the agent and prevent maternal and neonatal complications with high success rates
The incredible thing is that in the 21st century and in the world in general, less than half of pregnant women are cultivated to detect this germ and many are not even treated correctly, even knowing they are positive.
GBS in the mother
It causes uterine infections of varying severity. Endometritis, endomyometritis, infection of the operative wound, peritonitis. The vast majority of patients will respond adequately to treatment and mortality is very low if adequate care is established. Mortality in severe cases (septic shock, respiratory failure, meningitis and intractable tissue infection) could be estimated at 2% but depends on the health system responsible for the patient and their socioeconomic factors
GBS in the Newborn
Early start: <7 days
It occurs within the first 6 days after the birth of the baby and is due to the passage of bacteria to the amniotic fluid before delivery (chorioamnionitis) or neonatal contamination during vaginal delivery. 70% of the cases manifest the problem during the first 24-48 hours after birth: fever, lethargy, respiratory distress, jaundice, hypotension, pneumonia, meningitis. In 1977, neonatal mortality was 50% and currently it is estimated at 6%, depending on the health system and the experience in intensive care neonatal therapy.
Late start: 7 to 90 days
It occurs weeks after the birth with an average of 24 days and the most frequent manifestation (85%) is meningitis. It is not known exactly how the infection is acquired, its mortality is 10% and can leave neurological sequelae in up to 50% of babies
Is it then a terrible bacterium?
In fact it is a rather “stupid” bacterium since almost all the antibiotics of current use, and even many that have been stopped using due to bacterial resistance, are extremely effective; The fact is that most of the cases of neonatal infection by this bacterium can be prevented. What happens is that if we allow their entry into a weak individual the bacteria can make theirs and with little response to any antibiotic. I have never had a case of infection in mothers or newborns in 14 years of clinical experience
How can it be prevented?
This is very simple. A culture is taken from the anogenital region of the pregnant patient during week 35-37 of her pregnancy. If the culture is positive for GBS (10-30% of women), antibiotic treatment should be given during the entire duration of labor and until the baby is born. Whenever there are doubts, prophylactic antibiotic treatment can be started even without evidence of the presence of GBS
What treatment do I receive if I am a positive GBS?
None until delivery. This behavior calls the patient’s attention: how is it possible that if I have a bacteria in my body, my doctor does not treat me immediately with antibiotics? This seems strange but since the bacteria rarely affects the mother, no treatment is indicated; In addition, it was seen that those patients who were treated before the birth again colonized with the bacteria and when they went into labor with a doctor confident that the bacteria had been eradicated, the infection of the baby occurred.
If you are going to perform a cesarean, do I have to do the culture?
Yes. According to the latest guidelines for the management of GBS, all patients must be cultured because if a rupture of the membranes (water brake) occur before the caesarean section, the baby will become infected due to the rise of the bacteria through the defect. So, if I have a patient who goes for an elective cesarean section with a positive culture and one night she calls me saying that she has just broken water, the first thing I do is administer antibiotics to the mother to prevent bacteria ascension through the birth canal and avoid a fetal or neonatal infection and sepsis
Is the taking the sample bothersome?
Not at all, the sample is taken in 10 seconds by gently and superficially applying a sterile swab through the genital and anal areas. No need to use a speculum. The result will be given in 3-4 days.
Summary: the neonatal infection by GBS can be deadly for the baby but its prevention and management is extremely easy and effective, it is only necessary to cultivate the genito-anal area of the pregnant woman between weeks 35-37 and in case of being positive. Presence is administered the appropriate antibiotic during the entire process of delivery. The prevention of late infection is more difficult and less effective
Incidence and facts
Group B streptococcus causes, in the USA, approximately 1,200 cases of invasive disease of early onset each year, approximately 70% of them are full-term babies (after 37 weeks of gestation) and the case-fatality rate is 4% to 6%.
Mortality is higher among preterm infants, with a case-fatality rate of 20% to 30% for children born on or before 33 weeks of gestation
Where pregnant women undergo culture as part of their prenatal care, the incidence of early-onset GBS neonatal disease has markedly decreased
In Venezuela the statistics is worse due to the cultivation of less than 50% of pregnant women (the figure is unknown to the public and is very variable in the private sector, in my case it is 100%) and the limited resources of intensive therapy
Yates J – Centers for Disease Control and Prevention (CDC) has recommended screening and intra-partum prophylaxis among women who experience preterm labor, preterm premature rupture of membranes, group B Streptococcus in urine, and allergy to penicillin.
About 30% of healthy adult women are asymptomatic carriers of the germ. Outside of pregnancy, its presence does not matter.
Sampling procedure
A sample is taken with an applicator, gently rubbing the surface of the outer third of the vagina, inner side of the labia minor and the anal region and the sample is sent to the microbiology laboratory
