- Citas Centro Médico de Caracas: Lunes, Miercoles y Viernes. Pulse el botón Agende una Cita
- Sistema de citas en linea exclusivo para Centro Medico de Caracas en San Bernardino
- Citas CMDLT: Jueves. llamar al 0212-9496243 y 9496245
- Las Emergencias son atendidas en CMDLT previa coordinacion personal al 04142708338
- Proveedor Seguros Mercantil y Sudeban

Diabetes Mellitus is a chronic disease that is characterized by the presence of high levels of sugar (glucose) in blood (glycemia) due to a defect in the metabolism of carbohydrates and in the function or production of insulin. The degree of severity of diabetes has direct implications on the mother, the fetus and the general course of pregnancy.
Chronic hyperglycemia damages the arteries (macrovascular damage) and capillaries (microvascular damage) through the glycosylation or accumulation of irreversible products in the vascular walls of the arterial territory, affecting endothelial function, favoring the anomalous vascular growth (neovascularization), altering the capacity of vasodilatation, and exerting thrombogenic effects (chronic inflammation, platelet aggregation, fibrinolytic disorders and dyslipidemia) that obstruct the terminal circulation of the body’s most noble and susceptible tissues and organs (ischemia)
There are 4 types of diabetes (classification of the American Diabetes Association, 2007):
TYPE 1: (obsolete terms: Juvenile Diabetes, insulin-dependent diabetes) . This disease typically begins before age 30 and often presents acutely as uncontrollable appetite, high urinary frequency, dehydration, consciousness disorders, coma, etc. These patients are thin or very little overweight. The origin of this disease is due to the irreversible damage of the endocrine pancreas (apparently due to the effect of antibodies that attack it, autoimmune injury) with total abolition of insulin production. It has no hereditary component. The only valid treatment is the use of insulin. Represents 10% of diabetes cases
TYPE 2: (obsolete terms: Adult diabetes, non-insulin dependent diabetes) . It is a heterogeneous group of disorders characterized by varying degrees of insulin resistance, impaired insulin secretion, and increased glucose production. Due to the varied etiology it has, DM2 is susceptible to multiple treatments and preventive strategies. It represents 90% of diabetes cases. It usually begins after 30 years in patients with a tendency to overweight or obesity but due to the epidemic of overweight that is being experienced in the Western world we are seeing with an increasingly alarming frequency the appearance of type 2 diabetics at younger ages , under 30 years old, and incredibly in children up to 8-9 years old with overweight. It has hereditary character and with a more complex mechanism than Type1 but with a great association with overweight and obesity; Paradoxically, these patients may have a higher than normal production of insulin at some point, but their function is hampered by various mechanisms associated with excess body fat. Treatment includes diet, physical exercise, weight reduction, and blood sugar lowering medications taken orally. Occasionally and under certain conditions the type 2 diabetic may require insulin either intermittently or permanently.
In both types of diabetes the complications that can occur are the same: ocular, renal, nervous, cardiac and circulation damage of the limbs, especially the feet. The difference lies in the duration of diabetes, which is why type 1 presents them more frequently because it is an early onset disease. This is changing due to the new age of appearance of type 2.
Gestational diabetes: treated in depth in another article .
Diabetes of specific origin: Diabetes caused by mutations and specific defects of genetic, cellular, molecular, medicinal, endocrinopathological, infectious, etc. They are rare cases, some treatable when correcting the basic problem and other intractable ones that will require insulin for life
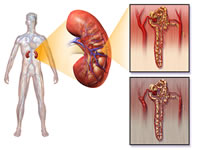
Microvascular manifestations of diabetes
Even when hyperglycemia affects the capillary system of all the organs of the economy, those that will be most affected are those that have very specialized terminal circulation. For example, the muscles have so much vascularity that their microcirculation, even when affected, is able to maintain the contractile function of the organ; However, organs such as the retina, peripheral nerves and kidneys are microvascularized with such specialization that they are not able to tolerate the chronic and progressive ischemia of uncontrolled hyperglycemia.
Diabetic retinopathy: Renitian damage is manifested by visual disorders and finally unilateral or bilateral blindness by complex mechanisms of ischemia, neovascularization and deposit harmful substances. In addition to this, cataracts and glaucoma may occur
Diabetic nephropathy: the terminal vascular damage in the kidneys affects the renal functional unit, the nephron. The progressive damage is manifested by loss of proteins and other substrates in the urine and the accumulation of waste substances giving rise to chronic renal failure to the point of completely losing kidney function and require dialysis to maintain life. Likewise, renal disorders lead to hypertension, lipid disorders and accelerated vascular damage, promoting the general complications of diabetes in all organs and systems.
Diabetic neuropathy: the restriction in the microcirculation that nourishes and oxygenates the peripheral nerves (vasa nervorum) leads to the dysfunction and death of the nerve terminals of many organs, generating disorders in the vegetative nervous function (cardiac, gastrointestinal, urinary disorders, erectile dysfunction ), sensitivity disorders in the feet and lower limbs (polyneuropathy), motor disorders / pain / weakness in the territory of a particular nerve (mononeuropathy)
Macrovascular manifestations of diabetes
In addition to hyperglycemia, lipid disorders are associated that accelerate vascular damage, particularly of the great arterial vessels, translating this into ischemic heart disease due to coronary injury, cerebrovascular accidents and peripheral vascular injury of the lower limbs that cause the so-called “diabetic foot” that can lead to gangrene and amputations.
I Effects of Diabetes on Pregnancy and the Fetus
In diabetic pregnant women, the most important problems are related to renal complications and an elevated risk of preeclampsia; In addition, the prognosis of pregnancy will depend on the presence of complications described above and this, based on the duration of the disease and its control during the evolution of it. The severity of the disease is inversely proportional to the reproductive success.
Insulin requirements will increase during pregnancy, especially between weeks 28-32, take your forecasts!
The patient will be evaluated every 1-2 weeks by their doctors (obstetrician, endocrinologist) until week 28-30 and then weekly until the end of pregnancy.
Maternal considerations
The duration of diabetes, daily glycemic control and microvascular and macrovascular damages define the potential complications that will manifest in pregnancy; No matter what they are, the end point is some type of hypertensive condition associated, produced or exacerbated by pregnancy.
The maxim is: the longer the disease and the worse the glycemic control, the greater the severity of maternal-fetal complications.
Hypertensive disorders: in pregnant diabetics the risk of suffering from preeclampsia/eclampsia is tripled or quadrupled (21-28%) in comparison with the normal pregnant woman (7%), this is particularly true in patients with nephropathy.
Preterm delivery: it is estimated that premature labor complicates diabetic pregnancy in 10-30% of cases (2-6 times higher than the general population), the figures are even higher in cases of poor glycemic control, diabetic complications and urogenital infections
Pyelonephritis: Symptomatic renal infection occurs in 4% of diabetic patients (several times more frequent than in the general population), perhaps due to high urine glucose values ??and urinary drainage disorders secondary to diabetic neuropathy
Fetal considerations
Congenital malformations: around 5% of fetuses of diabetic mothers will suffer some type of congenital malformation, tripling the expected global frequency (1.7%); however, it can reach up to 40% if the glycemic control of the disease was inadequate before pregnancy, especially if the glycosylated hemoglobin (HgbA1c, previous control marker -last 3 months- of glycemia, VN <6.5%) is greater than 9.3%. The congenital malformations mainly related to poorly controlled preconceptional diabetes are: congenital heart disease (transposition of large vessels, septal defects), malformations of the central nervous system (spina bifida, anencephaly and hydrocephalus), urinary malformations (renal agenesis, ureteral duplication and kidneys cystic), gastrointestinal malformations (anorectal atresia) and other less frequent (caudal regression syndrome). It is important to note that regaining strict control of glycemia before 10 weeks of pregnancy (organogenesis) reduces these risks
Abortion and early losses: It is possible that poor preconceptional glycemic control during early pregnancy increases the risk of miscarriage during the first trimester of pregnancy. The information is conflicting but it is not appropriate to tell a patient that she wants a pregnancy that does not strictly control her illness.
Late losses: there may be an increased risk of fetal mortality in late stages of pregnancy, especially in poorly controlled women during the third trimester of pregnancy. In addition, at this time it is possible that there are other adverse factors such as preeclampsia, placental insufficiency and oligohydramnios.
Macrosomia and Hyperinsulinemia: in hyperglycemic mothers without vascular damage the fetus receives loads of glucose (amino acids and fatty acids) extremely high so fetuses produce and maintain high levels of plasma insulin, manifest a high rate of growth and abnormally abundant accumulation of fat body (liver, abdomen, thighs). They are those “beautiful” babies weighing 5-6 kilos; beautiful, but potentially sick and susceptible to complications / trauma during birth and their first days of life (hypoglycemia, respiratory distress, hypocalcemia)
Prematurity: elevated as a consequence of the high risk of premature delivery / birth, either spontaneous or due to early termination of pregnancy by medical indication.
II Effects of Pregnancy on Diabetes
Pregnancy imposes new burdens on organs and they must withstand greater demands, if they are unable to comply with them, reversible or irreversible faults can occur in each of them. Rarely is deterioration so rapid and aggressive that pregnancy, regardless of fetal interest, must be interrupted to safeguard the life of the mother; however, this is uncommon.
Acute complications
Hypoglycemia : Inadequate intake, nausea and vomiting, especially during the first trimester, expose the patient to an increased risk of hypoglycemia due to the effect of variable doses of insulin and the tendency to rapid diabetic decompensation that pregnancy produces. The fetus is not affected by transient hypoglycemia in the mother.
Diabetic ketoacidosis during pregnancy (1-3%): feared complication inside and outside of pregnancy is due to acute diabetic decompensation due to inadequate treatment of diabetes (absent insulin or inadequate dosage), vomiting, infection, uteroinhibitors (B2 agonists used in threat of premature labor) and lung maturation with glucocorticoid steroids; All potentiated by the metabolic instability and insulin resistance of pregnancy. It usually occurs in the second / third trimester and can endanger the life of the mother (maternal mortality 4-15%) and the fetus (fetal mortality 9%). It is frequent in Type 1 Pregestational Diabetes but it can be seen in Type 2 and even in Gestational Diabetes. It requires acute treatment with high doses of insulin and hydroelectrolytic compensation in an emergency service, the fetus is in the background and their condition will be determined once the mother is compensated.
Chronic complications
Retinopathy: most studies indicate that diabetic retinopathy (one of the leading global causes of blindness in adults) progresses during pregnancy if the patient does not have strict glycemic control. Superimposed preeclampsia accelerates the progression of retinal damage. The patient must have an evaluation of the retina at the beginning of her pregnancy and as often as the specialist indicates if the patient has symptoms.
Nephropathy: 5% of diabetics suffer from diabetic nephropathy (glomerulosclerosis) during pregnancy and the degree of renal injury is associated with the frequency of maternal-fetal complications; in fact, pregnancy does not seem to accelerate the progression of the condition as long as the patient is managed by suitable specialists. For obstetricians this is one of the most feared situations, we are always waiting for the appearance of preeclampsia, placental insufficiency and retardation of fetal growth. The occurrence of hypertension and preeclamptic endothelial damage adds more kidney damage to diabetic nephropathy, Glomeruloendotheliosis, which exacerbates the loss of protein in the urine and may further decrease renal function (elevation of blood creatinine). As a general rule, renal function worsens irreversibly in 50% of patients, 25% worsens transiently and in 25% remains stable
Neuropathy and diabetic foot : the sensory damage in the lower limbs and the typical edema of pregnancy can further alter the healing in the diabetic patient with local traumas, it is imperative the proper hygiene, the care of the feet and the use of comfortable footwear and stable.
Macrovascular disease: patients with symptomatic vascular disease, especially in the coronary and cerebral territories, should be evaluated very carefully before deciding a future pregnancy since physiological changes of the vascular system during pregnancy can trigger complications such as heart attacks and thrombosis in their respective territories
Lab tests
*
1.-Diagnostic criteria of Diabetes Mellitus (types 1 or 2)
- Fasting blood glucose > 126 mg / dL
- Random blood glucose greater than 200 mg / dL
- Glycemia greater than 200 mg / dL at 2 hours after ingesting 75 g of glucose
Abnormal glycemia is not determined by a statistical value of population average as many medical values. It has been determined that starting from glycemias of 116 mg / dL the retina begins to be injured.
*
2.-glycosylated hemoglobin
- It is known as Hemoglobin HbA1c
- It is not recommended for diagnosis
- Normal value less than 6.5%
- It serves to verify historical adherence to treatment and fetal risk.
- Values ??greater than 7% are associated with congenital defects of the fetus, particularly heart disease.
Complications
Diabetic nephropathy: the microvascular damage injures the basic unit of the kidney, the Nephron.
Diabetic retinopathy: infarcts accumulation of abnormal material and formation of new arterial vessels that destroy the function of the retina.
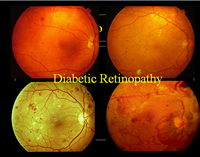
The retina of the asymptomatic patient must be evaluated at the beginning of her pregnancy, during the first trimester.
Diabetic foot : the dreaded ulcers due to minimal traumas.

Warning signs!
Symptoms of diabetic ketoacidosis in pregnant women:
- Polyuria: frequent urination
- Polydipsia: uncontrollable thirst
- Sickness
- Vomiting
- Abdominal pain
- Weakness
- Weightloss
- Loss of consciousness