- Citas Centro Médico de Caracas: Lunes, Miercoles y Viernes. Pulse el botón Agende una Cita
- Sistema de citas en linea exclusivo para Centro Medico de Caracas en San Bernardino
- Citas CMDLT: Jueves. llamar al 0212-9496243 y 9496245
- Las Emergencias son atendidas en CMDLT previa coordinacion personal al 04142708338
- Proveedor Seguros Mercantil y Sudeban

Toxoplasma gondii, an intracellular parasite, invades the cytoplasm of any nucleated cell and multiplies within it causing lesions in the tissues to which they originate, destroying the normal progression of the development of organs as important as the Brain
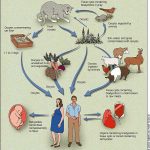
Toxoplasmosis can be transmitted via a transplacental route if the mother becomes infected during pregnancy, those infected before conception do not usually transmit toxoplasmosis to the fetus. The risk of transplacental infection increases from 15%, 30 and 60% when the mother is infected during the first, second or third trimester of pregnancy, respectively.
Parasitic infections are common in Africa, Asia, Central America, and South America, while relatively uncommon elsewhere.
In obstetrics, TORCH infections are important, which groups diseases produced by different parasitic (toxoplasmosis) and viral (rubella, cytomegalovirus, herpesvirus) agents that have in common the production of premature abortions and births, Perinatal infections with microcephaly-hydrocephalus, brain lesions, mental retardation or fetal death.
Massive serological examinations to the population indicate that human exposure to toxoplasmosis occurs worldwide and is common. The developing fetus and immunosuppressed patients experience special risk of severe disease.
The clinical manifestations of congenital toxoplasmosis are variable being characteristic the triad: hydrocephalus, intracerebral calcifications and Chorioretinitis. The diagnosis is established by serological tests. The parasite may be isolated during the acute phase of the disease, but this requires up to six weeks.
Infection can be avoided if raw or undercooked meat is not eaten. Specific treatment is indicated for acute toxoplasmosis of newborns, pregnant women and immunosuppressed patients. The most effective regimen is a combination of pyrimethamine plus sulfadiazine.
Epidemiology and pathogenesis
Interhuman contagion has not been described. It has been shown the possibility of acquiring toxoplasmosis also from transfusions of hematic products (total blood or leukocytes) from patients in phase of hematogenous dissemination or through transplanted organs containing Parasite cysts. Accidental inoculation has also been described in laboratory personnel. Tachyzoites can survive up to 50 days in total Citratada blood and kept at 4 °c, in other words, they can survive in blood stored in blood banks.
The main routes of transmission in humans are oral and transplacental.
Once ingested, the wall of tissue cysts, or oocysts sporulated, is destroyed by digestive enzymes, thus releasing the tachyzoites. These are disseminated via hematogenous or lymphatics after invading the cells of the intestinal epithelium and can reach any organ, although they are located especially in the skeletal muscle, the heart and the brain. The tachyzoites multiply in the inside of the cells and, when lysate, invade by contiguity the proximal cells and can remain viable during very prolonged periods inside the macrophages. The cessation of multiplication coincides with the emergence of the immune response (humoral and cellular). As a result, the tachyzoites are Encyst, a way in which they can remain viable throughout the patient’s lifetime. The proliferation of Tachyzoites can be extended more time in the CNS and in the retina of the patients, due to the difficulty of the antibodies to reach these locations or in case the infection occurs in an immuno compromised host. Reactivations coincide with transient or permanent depressions of cellular immunity.
Toxoplasmosis and Pregnancy
Congenital toxoplasmosis is transmitted by transplacental pathway and the necessary condition is that the mother suffers during the pregnancy a hematogenous dissemination. This occurs when the mother acquires a infection during pregnancy and, much more rarely, if as a result of an immunosuppression coinciding with the pregnancy a latent toxoplasmosis is reactivated.
This infection should take the placenta beforehand. The frequency of placentitis and the resulting fetal infection depends on the gestational age to which it occurs.
In the first quarter the percentage is 14%, 29% for the second and 59% for the third. Fetal contamination goes from 1% in the first quarter to 90% if it occurs during the third trimester. Fetal Parasitaemia is produced with diffusion of the parasite to the various tissues mainly retina, brain, muscle tissue, heart, liver, spleen and lung.
With the emergence of antibodies, cystic forms originate, which can invade and infect other organs.
The probability of a infection during pregnancy is 0.5-1%, irrespective of the geographic area. The overall probability of fetal transmission is 50%, although it appears to be considerably lower during the first trimester and higher during the last one, and can be reduced to 5% or less if the infection of the mother is detected and the treatment is administered Suitable. The overall incidence of Toxoplasma infection is 1-3 per 1,000 live births.
Pathology of intrauterine infection
In general, all chronic intrauterine infections are associated with intrauterine growth retardation. Being the symptomatic and fatal cases of infection of the first and second trimester. In late infection there is a greater likelihood of fetal infection but the damage is less. The neonate may therefore have a generalized disease or may have a predominant neurological compromise, or an isolated ocular compromise, as well as a latent form that manifests itself years later.
Almost all tissues may be compromised, muscle injuries are minor, while CNS and chorioretinitis lesions are of great importance
Zones of necrosis can affect the Aqueduct of Sylvio, the neural foramina and the cerebral ventricles originating hydrocephalus, or they can generate an intense inflammatory response, necrosis and severe cerebral and chorioretinitis calcifications associated to Multiple postnatal sequelae. Other organs affected can be the lungs, the digestive tract and mainly the liver, where it can produce cirrhosis, calcifications and jaundice. The newborn may manifest anemia, jaundice, thrombocytopenia, hepatosplenomegaly, and rash, simulating Neonatal Sepsis.
Diagnostic methods
Until the emergence of molecular biology techniques, the etiologic diagnosis of toxoplasmosis has been based, almost exclusively, on the detection of specific antibodies in serum, reserving mouse inoculation techniques and cell culture to Serious or potentially dangerous infections, such as acute infection in pregnant women, cerebral toxoplasmosis, and congenital infection.
Diagnosis of congenital toxoplasmosis in the newborn
Congenital toxoplasmosis is the result of fetal involvement as a result of maternal infection. The diagnosis of congenital toxoplasmosis is based on three distinct aspects: symptomatology, serological data and detection of the parasite or its DNA.
Newborn findings
The classic triad of congenital toxoplasmosis is the presence of Chorioretinitis, Hydrocephalus and Cerebral Calcifications. It is observed when the infection occurs in the first months of gestation and causes serious visual and neurological sequelae in the child. Other less frequent and specific signs that may appear in the newborn are jaundice, hepatosplenomegaly, thrombocytopenia, and Pleocytosis in the CSF.
Detection of the parasite or its DNA
It can be carried out according to the clinical situation, in the amniotic fluid and fetal blood during gestation, in the placenta after the birth and in the embryonic and fetal tissues in case of abortion or fetal death, in the newborn, in liver biopsy or in the LC R According to the symptomatology you present.
Serology
Maternal antibodies of the type IgG are transferred by the mother to the fetus, as they cross the Hematoplacentaria barrier. In non-infected newborn infants, these antibodies gradually decrease until they disappear between 6 and 12 months of life. In the newborn with congenital toxoplasmosis, the titer of antibodies can increase progressively and, in any case, these antibodies persist detectable beyond the 12 months of life.
Conclusions
In fact, it is not known exactly how many pregnant mothers are infected each year and what will be their long-term evolution, that is, what the consequences of toxoplasmosis in the social and professional life of infected children.
What still makes the early diagnosis of toxoplasmosis more difficult, is that most of the time it goes unnoticed in the pregnant woman because she is asymptomatic. Ignorance of the severity of the infection in the pregnant woman, for the fetus, leads to not being given the necessary importance, which brings disorders in the newborn, which makes it impossible in adulthood to lead an integral life with the consequent dependence of Third parties for their livelihood.
At the same time, it is worth saying that there is no control of free-living animals. It is therefore necessary to raise awareness among the population, especially pregnant women, to eat well-cooked meat, because as previously exposed, the cysts die by freezing at -20 º C or heating at 66 º C.
Also, it is not feasible to perform the deworming of cats, since the cysts in the soil are able to survive up to 18 months being constant sources of contamination.
Prenatal presumptive diagnosis is due to findings of unexpected neurocranial lesions during routine sonographic evaluation
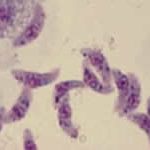
Toxoplasma gondii
Neonatal hydrocephalus associated with toxoplasmosis. This baby will require a surgical bypass to drain excess intracerebral fluid
Retinitis due to toxoplasma, follicular destruction of the retina (that area generates a blind spot in the visual field)
Starting from the contamination of soil and water the animals are infected by the ingestion of the eggs of the parasite (oocyte). The intermediate form of the parasite (tachyzoite) is able to cross the placenta and is responsible for fetal conditions.