- Citas Centro Médico de Caracas: Lunes, Miercoles y Viernes. Pulse el botón Agende una Cita
- Sistema de citas en linea exclusivo para Centro Medico de Caracas en San Bernardino
- Citas CMDLT: Jueves. llamar al 0212-9496243 y 9496245
- Las Emergencias son atendidas en CMDLT previa coordinacion personal al 04142708338
- Proveedor Seguros Mercantil y Sudeban

The Thyroid is an endocrine gland located in the lower part of the neck, is well known for its tumors (goiter) and the diseases that cause its dysfunction: Hypothyroidism (decreased function) and Hyperthyroidism (increased function, less frequent than the previous )
Hypothyroidism produces greater fetal problems than hyperthyroidism. In this article I develop primarily the first because it has practical and preventive tangible purposes.
This article was updated and changes were made (2017) due to the recently released American Thyroid Association (ATA) Guidelines: it is possible that the reference values of TSH may change, including the measurement of free T4 and antibodies antithyroid, make changes related to regions and ethnic groups.
In an article of March 2017, Treatment of Subclinical Hypothyroidism or Hypothyroxinemia in Pregnancy. Casey and Others | N Engl J Med 2017; 376: 815-825, treatment with thyroid hormone in pregnant women with subclinical hypothyroidism (TSH> 4.0 mUI / mL) did not generate cognitive benefits in children (up to 5 years) when compared with children of untreated women. Despite this, in my particular case, I will keep hormone therapy until this point is clarified better because its use is not contraindicated and the potential benefits outweigh the risks. In addition, treatment started relatively late and in many cases around week 20, this is why it is very important that the patient practice early prenatal studies to initiate thyroid supplementation before week 12 in cases in which TSH is greater than 4.0
Supplementation with selenium has no benefit in cases of hypothyroidism with positive antithyroid antibodies.
The product of the thyroid gland is the thyroid hormone, a protein compound formed by two molecules of the amino acid Tyrosine to which 3 or 4 molecules of Iodine are added: T3 (Triiodothyronine, 3 molecules of Iodine) and T4 (Tetrayodotironia or Thyroxine , 4 molecules of Iodo). The production of the gland is basically in the form of T4 and its peripheral conversion gives rise to the T3 that is the one that exerts the hormonal functions; thus, T3 is the active form of thyroid hormone. The commercial preparation of the hormone, levo- Tyroxin (Synthroid, Euthyrox) is a synthetic form of T4 that can be taken orally (preferably 60 minutes before lunch) and exerts its effect of thyroid hormone replacement by conversion to T3 in the tissues where it is necessary. T4 crosses the placenta and achieves certain fetal levels. T3 does not cross the placenta. The medication has an effect of 7 days so the dose changes should be made every 4-6 weeks. TSH measurements should be done in the same way every 4-6 weeks and it does not matter if the patient has taken the medication at the time of measurement (do not suspend the dose for that day).
Thyroid hormones act in almost all cells of the body, increase basal metabolism, affect the metabolism of proteins, fats, and carbohydrates, the growth of long bones and neuronal maturation. Thyroid hormones are essential for the development and proper differentiation of all cells of the developing human body during fetal life, especially for brain tissue
The fetus, even when it begins to produce thyroid hormones from week 12, depends on the thyroid hormones of the mother for its proper development and function.
This is why it is important to evaluate thyroid function at the first prenatal check-up.
Tests of thyroid function in pregnancy and its interpretation
During pregnancy the interpretation of normal values ??associated with thyroid function has changed. The hormone to be investigated is TSH (Thyrotropin, a hormone of pituitary production that is responsible for controlling the thyroid gland). The Trimester-Specific Reference Ranges for thyrotropin (TSH) have been reviewed and the following reference values ??are recommended:
First trimester 0.1 to 2.5 mUI/L
Second quarter 0.2 to 3.0 mUI/L
Third quarter 0.3 to 3.0 mUI/L
These values ??are being questioned and the current recommendation (2017) is to use 4.0 mUI L as a cut-off point to start treatment with T4 and it is expected that control levels will be maintained at less than 2.5 mIU/L during treatment . Based on these guidelines, corrections will be made.
The serum TSH provides the most accurate indication of the state of the thyroid in pregnancy, the measurement of T3, T4 and antithyroid antibodies is not practiced routinely and the interpretation is not so clear.
Hypothyroidism during pregnancy
Inefficient or subnormal thyroid function is by far the thyroid condition most frequently associated with pregnancy. Its counterpart, excessive function, hyperthyroidism, is rare.
The patient may present with known disease (Hypothyroidism) with or without treatment or have expressed TSH values ??higher than expected for the reference values ??of pregnancy. In both cases, the patient is usually asymptomatic and the object of treatment is to compensate thyroid function and prevent certain maternal-fetal complications:
1.-Abortion, habitual or recurrent abortion, prematurity, intrauterine growth retardation, in uterus fetal death, congenital anomalies, congenital hypothyroidism, infertility, preeclampsia, postpartum depression, postpartum hemorrhage.
2.-The most known and demonstrable risk is the defect in fetal brain development manifested in the postnatal period as a delay in psychomotor development, a decrease in the IQ and conduct disorders.
Hypothyroidism, whether symptomatic or asymptomatic, should be treated in pregnancy to prevent the risks described. This includes women with a TSH concentration above the specific reference range of the trimester.
The recommended treatment of maternal hypothyroidism is the oral administration of levo-thyroxine, the objective of normalizing maternal serum TSH values ??within the reference range for each trimester of pregnancy. The usual dose is 50 mcg per day and should be monitored by monitoring TSH levels every 4 weeks during the first half of pregnancy and at least once between 26 and 32 weeks of gestation.
After delivery, the medication should be reduced to the dose used before conception or the medication should be completely suspended for those patients who had values ??higher than 2.5 mIU/L but within the normal range for non-pregnant patients. Additional TSH tests should be performed approximately 6 weeks after delivery.
Hyperthyroidism during pregnancy
Excessive thyroid function is called hyperthyroidism. It is very rare in pregnancy, 1: 1000 pregnant. In more than 2 decades as a specialist I have only had 3 cases of hyperthyroidism associated with pregnancy, fortunately the behavior was adequate and there were no fetal problems due to the use of medications (Propylthiouracil, and Methimazole). The most frequent conditions are Graves’ disease and the presence of hyperfunctioning thyroid nodules. The risks to pregnancy and the fetus are less clear and frequent in this condition and we are concerned about their presence due to the potentially teratogenic effect of the available therapies.
If the hyperthyroidism is of immune origin, the thyroid stimulating antibodies can cross the placenta and stimulate the fetal thyroid, generating fetal goiter and hyperthyroidism (it is very rare and requires very high levels of maternal anti-thyroid antibodies). Drugs used in maternal hyperthyroidism (Methimazole and Propylthiouracil) can lead to fetal hypothyroid goiter and should be used in the lowest effective dose. This is the most frequent cause of clinically important fetal goiter and yet it is extremely rare 1 per 30,000 – 50,000 live births.

Fetal hypothyroid goiter in a mother treated with propylthiouracil (PTU), EXIT procedure: the newborn was intubated immediately at birth before cutting the umbilical cord to prevent asphyxia due to tracheal obstruction caused by the enlarged thyroid.
The thyroid
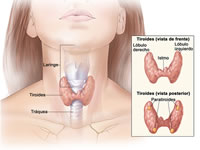
Located at the base of the neck, it is usually not very palpable at the sternum fork.
Endocrine control

The thyroid is controlled by the pituitary gland through a hormone called TSH (Thyroid Stimulating Hormone) or Thyrotropin. The measurement of TSH levels gives us a clear idea of ??the functioning of the gland and allows us to talk about Hypothyroidism (decreased function), Hyperthyroidism (excessive function) or Euthyroidism (normal function). The pituitary gland is, in turn, controlled by a hormone of cerebral origin (hypothalamus) called HRT, but it has little clinical utility.
T4: tetraiodothyronine
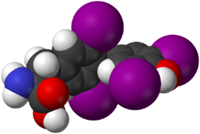
The T4, form of secretion of the thyroid hormone, is a pro-hormone with little activity that must be converted into T3 to exert its effect at the tissue level. Its measurement provides data on the global function of the gland. Its free portion is biologically active and is 0.03% of the total T4 concentration.
T3: triiodothyronine
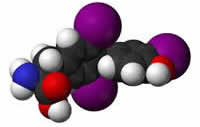
T3 is the active form of thyroid hormone, comes from the elimination of a molecule of Iodine of T4 which makes it very active in almost all tissues of the body.
Iodo
The iodine is the primordial element of the thyroid hormone and necessary for its synthesis and function. Deficit of Iodus can lead to Hypothyroid Goiter.

The iodized salt has prevented the appearance of goiter due to insufficient intake of water in almost all the world. Iodine requirements increase in pregnancy due to increased hormonal production and greater renal loss.