- Citas Centro Médico de Caracas: Lunes, Miercoles y Viernes. Pulse el botón Agende una Cita
- Sistema de citas en linea exclusivo para Centro Medico de Caracas en San Bernardino
- Citas CMDLT: Jueves. llamar al 0212-9496243 y 9496245
- Las Emergencias son atendidas en CMDLT previa coordinacion personal al 04142708338
- Proveedor Seguros Mercantil y Sudeban

During pregnancy, there are multiple and varied fetal problems that can occur. In this article we expose some of the most common, its meaning, related basic concepts and demystify some misconceptions.
I Placenta “aged”
This is an inappropriate term since it suggests weak or senescent function of the placenta without considering its actual functionality. It is based on the visual identification of placental calcification in degrees not according to the gestational age of pregnancy; In short, it is more calcified than expected for the time of pregnancy. In modern practice most of the placentas “aged” or prematurely mature do not represent any problem because the Doppler evaluation of the arteriovenous circulation of the umbilical cord allows discarding them, leaving this ancient visual concept without effect. Placental grade is not valid for making obstetric decisions in the absence of fetal Doppler evaluation.
II Oligoamnios (0.5-1% of pregnancies)
It is the decrease of the amniotic fluid (liquid index less than 5 cm according to the ultrasound measurement called Amniotic Liquid Index or ILA). Its importance lies in the increasing rates of fetal morbidity and mortality with decreasing levels of amniotic fluid
The fluid decreases due to lack of fetal production (basically the baby does not urinate -the most frequent-) or genital loss through some orifice in the amniotic sac (RPM, premature rupture of membranes), the first is progressive and does not carry a risk of infection and the second is usually abrupt and irreversible due to the onset of labor and / or the intractable infection that eventually occurs (7-14 days).
Most cases are late and easily managed with excellent neonatal prognosis, many are due to maternal dehydration. Occasionally, oligohydramnios is present early (before week 24) and fetal pronostomy is very bad due to fetal crush deformities (Potter syndrome), associated fetal anomalies (kidneys and urinary tract), severe circulatory problems (early placental insufficiency , retardation of fetal growth) and the inevitable infection (in cases of RPM).
The initial indication in the absence of findings that explain it is the correction of maternal hydration through the intake of water without other additives. The use of coconut water is recommended but I believe that its effect is due to the free water content and I think it can be risky if the source is contaminated or aged on a supermarket shelf.
Overhydration test: to demonstrate that the decrease in amniotic fluid is due to maternal dehydration, you will be asked to drink 2 liters of water in a period of 2 hours and you will have an ultrasound when you finish drinking the water. An increase of approximately 30% of the volume is expected. If there is vomiting or the oral route is not tolerated, intravenous solutions will be used to perform the test
III Polyhydramnios (0.5-1% of pregnancies)
It is the abnormally high accumulation of amniotic fluid (fluid index greater than 24 cm according to the measurement of the Amniotic Liquid Index or ILA) due to an excess of fetal production (fetal urine) or the lack of fetal swallowing of the amniotic fluid that is its main regulatory mechanism. In almost all cases the event is innocuous (idiopathic, of unknown cause, 90%) and has a tendency to spontaneous resolution due to fetal maturation. The remaining 10%, the rare cases caused by placental tumors, maternal diabetes, structural fetal lesions, fetal anemia, fetal neuromotor disorders and multiple pronotic pregnancy are variable and occasionally very reserved. Amniocentesis (Amnioreduction) to reduce fluid is reserved for those cases in which the cervix is ??less than 15 mm or serial follow-up reports progressive reduction of the cervical length below 25 mm (to prevent premature delivery )
IV Premature rupture of membranes (RPM)
It refers to the rupture of membranes before the start of labor; In addition, if the break occurs before 37 weeks, the condition is called Pretreatment Pretreatment of Membranes (RPPM) . The immediate problem of PROM is infection and labor. If the MPR occurs after week 37 (full-term fetus), it continues with the birth of the baby, if it occurs between weeks 34-36 it is possible that the obstetrician indicates the interruption of the pregnancy. In RPPM far from the term (weeks 24-34), an attempt will be made to keep the fetus in the womb until the labor begins or the liquid is completely depleted or an infection ensues. In RPPM before week 24 the fetus is not viable and the decision to interrupt or maintain the pregnancy and then give some kind of attention to the aborted or premature fetus will depend on gestational age and fetal weight
The neonatal prognosis will depend on the gestational age, the presence of infection and the effectiveness of the Neonatal Intensive Care Unit. The prognosis is poor (or non-existent from a practical point of view) before week 24 due to the absence of structurally formed lungs.
V Fetal distress (SF)
This is a broad term that refers to the alteration of fetal health tests, they are translated into alterations in fetal nutrition and oxygenation. It is associated with decreased fetal movements and amniotic fluid and long-term fetal growth. Unattended and adequate measures could lead to fetal death. Acute (SFA) refers to acute fetal oxygenation disorders during labor, maternal hemorrhages, placental abruption, cord accidents, etc. Chronic (CFS) , chronic and progressive decrease of fetal oxygenation and nutrition, the fundamental manifestation is the restriction of fetal growth (IUGR)
VI Umbilical Cord Circulars and Fetal Death
There is no evidence that cord circulars hang / choke / kill the fetus during normal pregnancy. It is expected that up to 40% of the fetuses have cord circles. Doppler of the umbilical artery demonstrates the absence of circulatory effects in the fetus carrying one or more cord circulars in the absence of fetal circulatory disorders. Circulars are important in vaginal delivery, by traction and strangulation, if the turns are too tight and the cord is too short but this is identifiable and only leads to cesareans or simple maneuvers during vaginal delivery. Particularly I have attended deliveries with 4 rounds of cord without any problem, in some cases I had to suspend delivery and perform an emergency cesarean (without complications) fetal heart rate disorders (SFA) probably related to the cord.
I do not believe the story that the baby died (drowned, strangled) by cord circles during pregnancy: surely there was a fetal circulatory problem, placental insufficiency or undiagnosed fetal malformation
VII Fetal death in utero
This is a relatively rare tragedy and almost invariably of known cause. The most frequent causes are chromosomal disorders, genetic syndromes, major congenital malformations, placental insufficiency, hypertensive disorders of pregnancy, maternal autoimmune diseases with placental vascular effects, etc. In 20 years of experience (and counting) as a specialist I have only had one case of fetal death (21 weeks) without any data – sonographic, circulatory, bacteriological, anatomopathological, immunological – that explains it.
Circular double cord: this image shows double circular in a healthy fetus; pregnancy and childbirth without complications.

Polyhydramnios: increased amniotic fluid, in this case a vertical pocket greater than 10 cm ( Clin Invest Ginecol Obstet, 2012; 39: 132. Sanchez T et al.)

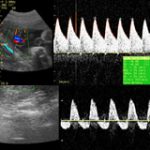
Fetal Doppler: this image shows two studies (umbilical cord Doppler), one with normal umbilical circulation and another with severe (lower) involvement. The compromised case was interrupted in 48 hours, after maturing lungs with betamethasone and monitoring every 24 hours.
*
Fetal Health Tests: Fetal Biophysical Profile, PBF (Manning et al.)
This is an abstract concept that includes relatively objective schemes related to fetal health to determine the survival / mortality / morbidity in utero of a committed fetus
The most used, after week 32, is the Fetal Biophysical Profile (PBF, Manning et al 1985) which includes 5 parameters: Variable heart rate (Fetal monitor), Respiratory movements (Echo), Body movements (Echo), Flexion and extension (Eco), Amniotic fluid (Eco). Each parameter has two values, 0 and 2 and the sum of the values ??obtained gives a final score that suggests fetal mortality in the next 7 days. The full PBF includes Electronic Fetal Monitoring to determine the fetal heart rate and its characteristics of variability with a total score of 10/10 in a healthy fetus. The abbreviated PBF (the one we use the most) only considers the sonographic elements for a score of 8/8
Interpretation: mortality according to the results
8/8 , mortality in 7 days 0.08%
6/8 , mortality in 7 days 0.9%
4/8 , mortality in 7 days 2.6%
2/8 , mortality in 7 days 9.4%
0/8 , mortality in 7 days 28.5% (some report 60%)
What does the alteration in the PBF mean?
Potential disorders of fetal organic development by disruption of cellular physiological processes by hypoxia and lack of fetal nutrition
Fetal Health Tests: Fetal Doppler
The evaluation of the fetal circulation by pulsed Doppler or Pulsed Color Doppler, starting at week 24, allows us to identify early those fetuses that face placental dysfunction, even before they manifest alterations in the PBF described above. It also allows us to differentiate babies with growth problems (Intrauterine Growth Delay -RCIU-) from those small babies due to parental inheritance (small constitutional), genetic vs. placental causes in growth disorders and to determine with the help of the PBF the most suitable for the termination of pregnancy before they supervene complications or fetal death